
Antibacterial Sutures Reduce Costs and Risks of SSIs
Surgical Site Infections (SSIs) continue to be one of the most common and costly healthcare-associated infections – with potentially catastrophic consequences to patients. Despite significant advances in the area of wound closure and healing, SSIs still occur in up to five percent of patients undergoing surgery1-3 and the results can be life altering.
In the United States alone, there are more than 300,000 cases of SSIs occurring each year3. Those who are impacted by SSIs increase their length of hospital stay by up to 11 days1, 3, are five times more likely to be readmitted to the hospital1 and two times more likely to spend time in an intensive care unit1. A single SSI can cost up to $39,0004, costing the healthcare system an additional $3.5 to $10 billion annually1-3. These numbers are staggering.
The sad reality is that we see the catastrophic impacts of SSIs far too often.
In 2006,
SSIs are challenging for physicians to address since they can happen from varying types of surgeries at the hands of the most skilled surgeons. The good news is – SSIs are preventable and there are proactive measures that healthcare professionals can take to reduce the risk of these infections. However, it is up to each and every medical professional to mitigate these risks. Here are some proactive measures OR staff can take to provide extra risk reduction…
- Implement tools, like a surgical safety checklist or environmental cleaning protocols, that allow the OR staff to manage SSI risk factors more proactively. Vocalize concerns if a break in proper sterilization occurs and correct the error immediately.6
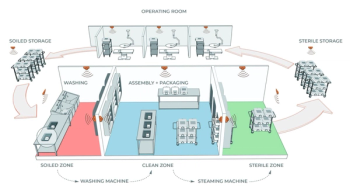
- Mitigate risks where nurses and surgeons have control by cleaning hands often with alcohol-based products, minimizing traffic in the operating room and wearing scrubs that have been laundered by the facility.6
- Develop SSI prevention strategies and share this information with patients prior to surgery, especially if they are immunosuppressed and they or their family have previously experienced SSIs.6
Another way to mitigate risks is to use Ethicon’s
Using antibacterial sutures is a simple choice that gives physicians the power to reduce a persistent risk from the surgical equation. They add an extra layer of protection for patients, and it’s simple to implement into surgical procedures. Triclosan-coated sutures should be an indispensable component of every operating theater’s infection prevention protocol to ensure medical professionals are using technology to address as many known SSI risk factors as possible.
In addition to using an antibacterial suture, there is another wound closure option that avoids the risk factor of suture colonization by bacteria– and that is skin closure without sutures, a mesh reinforced topical skin adhesive, which closes the surgical incision at every point along its length.
The bottom line is—SSIs are a global healthcare concern that needs to be addressed more widely. One surgical site infection is one too many. As we forge ahead, together, antibacterial sutures and additional proactive infection prevention protocols can one day take us to a world where SSIs are a thing of the past. Learn more about these proactive surgical site infection prevention protocols and join the
*In a meta-analysis of 21 RCTs, 6462 patients, 95% CI: (14, 40%), P<0.001
†All triclosan-coated sutures in these RCTs were Ethicon Plus Antibacterial Sutures (MONOCRYL® Plus, VICRYL® Plus, and PDS® Plus)
References:
- World Health Organization. WHO Guidelines for Safe Surgery, 2009.
- Thompson KM, Oldenberg WA, Deschamps C, Rupp WC, Smith CD. Chasing zero: The drive to eliminate surgical site infections. Ann Surg. 2011;254:430-437.
- Anderson DJ, Podgorny K, Berrios-Torres SI, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(6):605-627.
- de Lissovoy G, Pan F, Patkar A, et al. Surgical Site Infection Incidence and Burden Assessment Using Multi-institutional Real-world Data. Presented at EU ISPOR, 2011, Madrid, Spain.
- de Jonge SW, Atema JJ, Solomkin JS, Boermeester MA. Meta-analysis and trial sequential analysis of triclosan-coated sutures for the prevention of surgical site infection. Brit J Surg. 2017;ePub-DOI: 10.1002/bjs.104-45.
- Spruce, L. (2014), Back to Basics: Preventing Surgical Site Infections. AORN Journal, 99: 600-611. https://doi.org/10.1016/j.aorn.2014.02.002.
- Berríos-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. doi:10.1001/jamasurg.2017.0904.
- WHO Global Guidelines for the Prevention of Surgical Site Infection, 2016.
- Ban KA, Minei JP, Laronga C, et al. American College of Surgeons and Surgical Infection Society: Surgical Site Infection Guidelines, 2016 Update. J Am Coll Surg. 2016;224:59-74.
193014-211020
© Ethicon Inc. 2021
Newsletter
Stay prepared and protected with Infection Control Today's newsletter, delivering essential updates, best practices, and expert insights for infection preventionists.
Related Content



Safeguard your facility with high-performance facial protection
