Closing the Gap: Maximizing the Potential of UV-C Technology to Reduce Health Care-Associated Infections
Effective implementation of UV-C disinfection is crucial to reducing HAIs. The Providence Holy Cross Medical Center achieved a 19% reduction in multidrug-resistant HAIs and saved $1.2 million through strategic deployment, highlighting the importance of collaboration and innovative management.
An artistic 3D illustration of a hospital room with virus particles in the air, showcasing the importance of proper hygiene and infection control in health care.
(Adobe Stock 853610624 by MAY)

Reducing pathogens in a patient environment lowers health care-associated infections (HAIs),1 and UV-C surface disinfection reduces pathogens in a patient environment.2 So why are epidemiologists not always confident that UV-C will reduce HAIs in their hospital?
Effective UV-C implementation is poorly understood.3
To fulfill the HAI-fighting potential of UV-C surface disinfection devices, hospitals must focus on implementation. The challenge posed by UV-C devices is using them frequently and strategically enough to successfully reduce HAIs without disrupting hospital operations–and a California hospital may be the template.
After 1 year of the Providence Holy Cross Medical Center (PHCMC) UV-C program, the hospital had reduced multidrug-resistant HAIs by 19%. It saved over $1.2 million by avoiding excess HAI-related inpatient days without adversely impacting emergency room (ED) admissions,4 providing a net financial benefit to their institution while improving patient outcomes. Their results were achieved through innovative program management and a clear assignment of roles among the hospital leadership, the service providers, and the technology providers.
The breakdown of responsibility among the stakeholders is as follows:
Hospital Leadership
● Choose how the UV-C program is staffed, ie, hire the service providers. Most hospitals use environmental services (EVS) technicians; however, PHCMC contracted a team of dedicated operators from Clean Sweep Group, Inc (CSGI) with previous experience implementing UV-C. The decision had 2 primary benefits.
First, PHCMC did not undergo an extended experimentation period and failed policies. The service provider used practices and staff already proven in other hospitals and adapted them to the hospital leadership’s policies and goals. This ensured PHCMC a robust UV-C program on day 1.
Second, operational knowledge was better preserved with a dedicated service provider, and the UV-C program is better protected from quality degradation due to staff turnover.
Health care-associated infections by Infection Control Today

● Adopt a flexible policy to minimize disruption of patient flow but maximize opportunities to use UV-C. At PHCMC, hospital leadership concluded UV-C can be used in any clinical space within the hospital with the caveat that a patient's admission could not be extended more than 5 minutes due to the extra cleaning step required for UV-C disinfection. The policy dramatically expanded the number of opportunities to use UV-C, but more importantly, hospital operations were not disrupted. Rigid policies dictating certain rooms must always be UV-C disinfected, while others may not limit the efficacy of UV-C programs and inhibit patient flow.
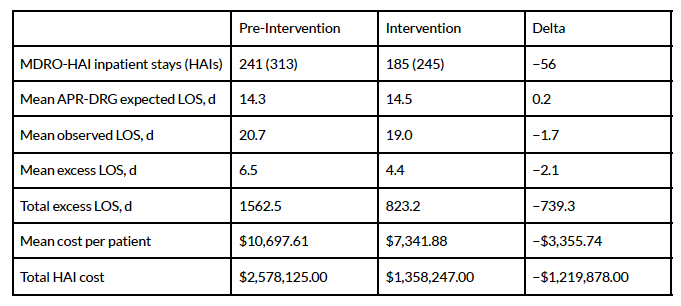
● Identify UV-C program goals and metrics. PHCMC sought to reduce HAIs while breaking even on the cost of the program by factoring in the direct cost of HAIs. The direct cost of HAIs was calculated by determining the excess length of stay attributable to the HAI and multiplying it by the hospital’s average cost for patient services per day. A simple tally of the preintervention and intervention periods determined that PHCMC saved over $1.2 million over a 1-year intervention (Figure 1)4 and had positive net cost savings from the UV-C program because of reduced HAIs.
Figure 1. 12-month Pre-Intervention (No UV-C) and Intervention (With UV-C) period direct cost associated with multidrug-resistant organisms (MDROs) HAIs.
(Figure credit: Authors; data from Raggi et al.)
The role of hospital leadership–ie, infection preventionists, nursing leadership, and the C-Suite—role is summarized as providing the people, policies, and metrics of a successful UV-C program. However, it is the role of the service providers to actualize the program.
Service Providers
● Develop a deployment protocol to meet hospital leadership’s goals. Per PHCMC UV-C policy, all clinical spaces–eg, inpatient discharges, procedural spaces, and emergency rooms–are considered potential targets for disinfection. To accommodate this wide scope, the service provider implemented a triage protocol with the following priorities:
i. critical inpatient spaces,
ii. scheduled spaces,
iii. non-critical spaces. If a space in the tier above is not available for disinfection, the service provider moves to a lower tier option and revaluates after completion of every disinfection. Given that many hundreds of potential spaces need to be disinfected, the service provider uses CSGI Triage software to manage this complex protocol. Implementation of a hospital-wide triage protocol was associated with a 19% reduction in HAI incidence rate at PHCMC, while the isolation-only protocol in the BETR trial achieved an 11% risk reduction.4,5
● Maintain quality standards and monitor program metrics. The service provider’s software collated hospital data and log information generated by the UV-C device to monitor protocol compliance and deliver automated reports to hospital leadership. Detailed analytics per UV-C device and technician are available to quickly identify and correct issues.
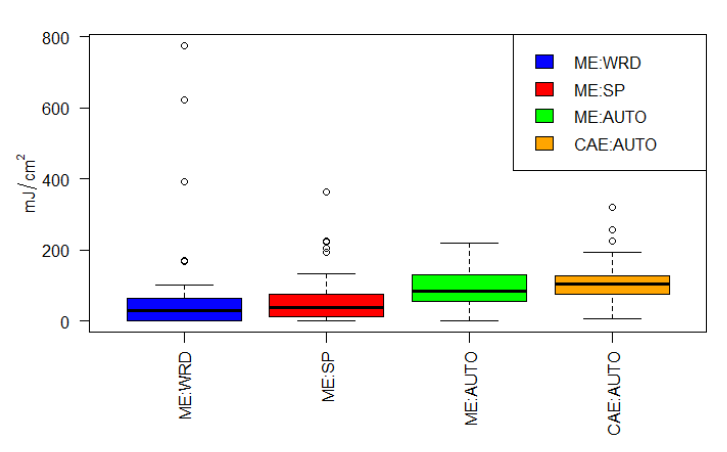
● Choose the UV-C technology, ie hire the technology provider. The service provider at PHCMC periodically reevaluates UV-C technologies and, with the consent of hospital leadership, may adopt new devices if warranted. After the introduction of autonomous UV-C devices, the service provider and PHCMC’s hospital leadership compared autonomous positioning strategies with whole-room and spot strategies.
An autonomous strategy produced significantly higher UV-C dosages (85.1 mJ/cm2) compared to whole-room (29.02 mJ/cm2) and spot disinfection (37.83 mJ/cm2) placement strategies
(Figure 2)6 The analysis determined adoption of a new technology was justified, and the service providers selected the OhmniClean semi-autonomous UV-C robot by OhmniLabs in Milpitas, California.
Figure 2. Boxplot of UV-C dosages achieved with a control emitter (ME) using whole-room (WRD), spot (SP), and autonomous (AUTO) positioning strategies alongside a commercially available autonomous device (CAE).
(Figure credit: authors; data from Haag et al.)
The service provider determines the most effective method of deploying hospital leadership’s UV-C program framework, including room prioritization, monitoring, and UV-C technology. The technology provider supplies the service providers with the necessary hardware and support to complete their responsibilities.
Technology Providers
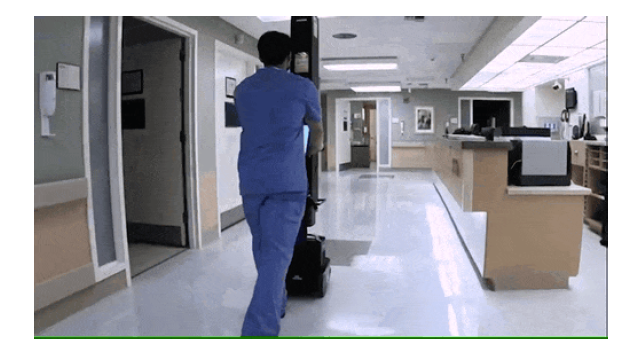
● Outcompete other UV-C technologies. Among the cohort of autonomous devices, the service providers at PHCMC chose the UV-C device based upon i. a small footprint, ie ability to maneuver within a crowded patient room and access to conjoined patient bathrooms, and ii. unlimited device uptime enabled by a swappable external battery, which is critical for reducing the UV-C technology cost.
Figure 3. Demonstration of OhmniClean’s maneuverability in complex environments and ability to disinfect conjoined rooms, eg a patient bathroom, within 1 cycle.
(Image credit: authors.)
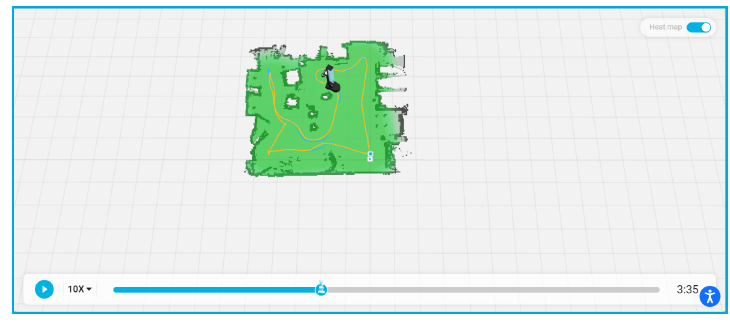
● Data sharing with service providers. The service provider’s software automatically ingested data from the UV-C devices at PHCMC. This data-sharing practice enables various enhanced management and quality control capabilities. In addition, a 2D map generated by the onboard LIDAR system visualized the device's movement throughout the disinfected space, providing the service provider with unprecedented oversight of the disinfection process.
Figure 4. OhmniClean Light Detection and Ranging (LIDAR) map displaying the robot’s disinfection path throughout the target space. A time-lapsed map is generated for every disinfection.
(Figure credit: authors and OhmniClean)
● Provide timely service and repair. Through consistent communication and detailed analysis of device logs, operational issues with the device are quickly identified and resolved. As a result of this collaborative effort, the UV-C program has not had a single day without completed disinfections since the adoption of the UV-C device at PHCMC. Technology providers equip the service providers with tools to carry out their functions, and the support to maintain the continuance and quality of the UV-C program.
Summary
The HAI-fighting potential of UV-C robots has been largely unrealized as institutions have focused on technology and overlooked strategic deployment. More substantial health and financial benefits have yet to be realized, but they are coming. PHCMC’s focus on strategic implementation, including innovative management, a triage UV-C disinfection protocol, and technology partner collaborations, is maximizing the HAI-fighting potential of UV-C.
References
1. Datta R, Platt R, Yokoe DS, Huang SS. Environmental cleaning intervention and risk of acquiring multidrug-resistant organisms from prior room occupants. Arch Intern Med. 2011 Mar 28;171(6):491-4
2. Rutala WA, Gergen MF, Weber DJ. Room decontamination with UV radiation. Infect Control Hosp Epidemiol. 2010 Oct;31(10):1025-9
3. Schaffzin JK, Wilhite AW, Li Z, Finney D, Ankrum AL, Moore R. Maximizing efficiency in a high occupancy setting to utilize ultraviolet disinfection for isolation rooms. Am J Infect Control. 2020 Aug;48(8):903-909
4. Raggi R, Archulet K, Haag CW, Tang W. Clinical, operational, and financial impact of an ultraviolet-C terminal disinfection intervention at a community hospital. Am J Infect Control. 2018 Nov;46(11):1224-1229
5. Anderson DJ, Moehring RW, Weber DJ, Lewis SS, Chen LF, Schwab JC, Becherer P, Blocker
M, Triplett PF, Knelson LP, Lokhnygina Y, Rutala WA, Sexton DJ; CDC Prevention
Epicenters Program. Effectiveness of targeted enhanced terminal room disinfection on hospital-wide acquisition and infection with multidrug-resistant organisms and Clostridium difficile: a secondary analysis of a multicentre cluster randomised controlled trial with crossover design (BETR Disinfection). Lancet Infect Dis. 2018 Aug;18(8):845-853
6. Haag CW, Holliday G, Archulet K, Tang W. Comparing UV-C dosages of emitter placement strategies in a community hospital setting. Infect Control Hosp Epidemiol. 2023 Sep;44(9):1505-1507
Newsletter
Stay prepared and protected with Infection Control Today's newsletter, delivering essential updates, best practices, and expert insights for infection preventionists.
Reducing Hidden Risks: Why Sharps Injuries Still Go Unreported
July 18th 2025Despite being a well-known occupational hazard, sharps injuries continue to occur in health care facilities and are often underreported, underestimated, and inadequately addressed. A recent interview with sharps safety advocate Amanda Heitman, BSN, RN, CNOR, a perioperative educational consultant, reveals why change is overdue and what new tools and guidance can help.
New Study Explores Oral Vancomycin to Prevent C difficile Recurrence, But Questions Remain
July 17th 2025A new clinical trial explores the use of low-dose oral vancomycin to prevent Clostridioides difficile recurrence in high-risk patients taking antibiotics. While the data suggest a possible benefit, the findings stop short of statistical significance and raise red flags about vancomycin-resistant Enterococcus (VRE), underscoring the delicate balance between prevention and antimicrobial stewardship.
What Lies Beneath: Why Borescopes Are Essential for Verifying Surgical Instrument Cleanliness
July 16th 2025Despite their smooth, polished exteriors, surgical instruments often harbor dangerous contaminants deep inside their lumens. At the HSPA25 and APIC25 conferences, Cori L. Ofstead, MSPH, and her colleagues revealed why borescopes are an indispensable tool for sterile processing teams, offering the only reliable way to verify internal cleanliness and improve sterile processing effectiveness to prevent patient harm.
The Next Frontier in Infection Control: AI-Driven Operating Rooms
Published: July 15th 2025 | Updated: July 15th 2025Discover how AI-powered sensors, smart surveillance, and advanced analytics are revolutionizing infection prevention in the OR. Herman DeBoard, PhD, discusses how these technologies safeguard sterile fields, reduce SSIs, and help hospitals balance operational efficiency with patient safety.
Targeting Uncertainty: Why Pregnancy May Be the Best Time to Build Vaccine Confidence
July 15th 2025New national survey data reveal high uncertainty among pregnant individuals—especially first-time parents—about vaccinating their future children, underscoring the value of proactive engagement to strengthen infection prevention.