
News




For the past 15 years, Erika Garcia has worked for the World Health Organization (WHO) as an infectious disease control specialist. Erika has been deployed for a variety of disease outbreaks, including Middle East Respiratory Syndrome Coronavirus in Qatar and an unknown cause of illnesses and deaths in Panama that was later characterized as renal failure syndrome due to consumption of contaminated medications, among others.



There have been no MERS cases in the United States since May 2014, and the Centers for Disease Control and Prevention (CDC) says the risk of MERS to the general public in this country remains very low. The CDC and other public health partners continue to closely monitor the MERS situation.





Between June 5 and June 8, 2015, the National IHR Focal Point for the Kingdom of Saudi Arabia notified the World Health Organization (WHO) of eight additional cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection

The Centers for Disease Control and Prevention (CDC) will offer a Grand Rounds session, "Working to Eliminate Measles Around the Globe," on Tuesday, June 16, 2015 at 1 p.m. ET.

On June 10, 2015, the National IHR Focal Point of Chile notified the World Health Organization (WHO) of five cases of measles infection.


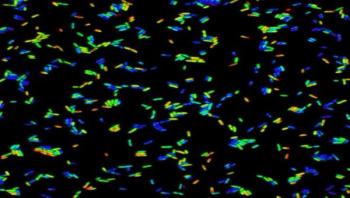
A new, rapid method is helping detect how bacteria sense and respond to changes in their environment. Bacteria can pick up external signals, which then relay to internal signaling pathways that direct their behavior. This surveillance also can trigger survival tactics for a variety of harsh situations, such as lack of nutrients or the presence of antibiotics. In a cover article published June 9 in Science Signaling, microbiologists expressed particular interested in the sensing done by the food-poisoning bacteria, Salmonella. The pathogen is adept at adjusting to different locations and surrounding conditions. One of its safety strategies is to gather into a biofilm -- a collection of bacteria huddled together in a protective coating.





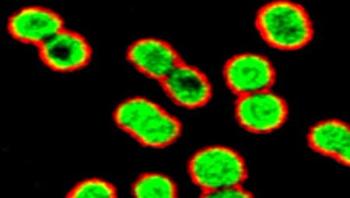
Researchers at Queen’s University Belfast have developed a cutting-edge new medical therapy that could protect UK hospital patients against a lethal superbug. The new treatment, which uses a molecule called an inhibitor to prevent the hospital superbug Klebsiella pneumonia from blocking the body’s natural defenses, has the potential to save thousands of lives in the UK each year. Klebsiella, which has mortality rates of 25 percent to 60 percent, can cause bladder infections and pneumonia and is resistant to all major antibiotics.
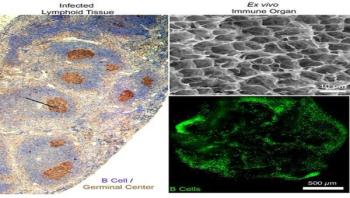
Cornell University engineers have created a functional, synthetic immune organ that produces antibodies and can be controlled in the lab, completely separate from a living organism. The engineered organ has implications for everything from rapid production of immune therapies to new frontiers in cancer or infectious disease research.
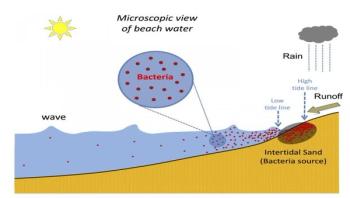
An international team, led by researchers at the University of Miami (UM) Rosenstiel School of Marine and Atmospheric Science, has developed a new, timelier method to identify harmful bacteria levels on recreational beaches. The new model provides beach managers with a better prediction tool to identify when closures are required to protect beachgoers from harmful contaminates in the water.
Contrary to current medical dogma, researchers at University of California, San Diego School of Medicine and Skaggs School of Pharmacy and Pharmaceutical Sciences report that the common antibiotic azithromycin kills many multidrug-resistant bacteria very effectively -- when tested under conditions that closely resemble the human body and its natural antimicrobial factors. The researchers believe the finding, published June 10 by EBioMedicine, could prompt an immediate review of the current standard of care for patients with certain so-called "superbug" infections.

This special digital issue reviews the many occupational hazards in the healthcare laundry environment and explores how to protect hospital laundry personnel from sharps injuries and bloodborne pathogen exposures.

This collateral material describes Aramark's MicroVantage process in which the company launders its microfiber products with a sanitizer that protects fibers while eliminating 99.9 percent of pathogens. The MicroVantage process is step one of Aramark's innovative four-step system.