News
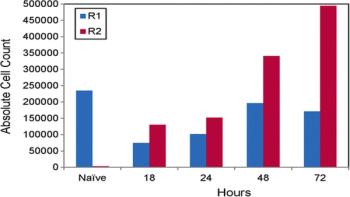
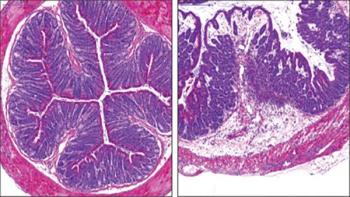
A new study of infection by a virus that causes brain inflammation and seizures in a mouse model has shown increased levels of complement component C3. The C3 was produced by immune cells in the brain called microglia within the first few days after infection. C3 showed the greatest increase in expression in the brain compared to a variety of other complement components, cytokines, chemokines, and antigens measured in the study that is published in Viral Immunology, a peer-reviewed journal from Mary Ann Liebert, Inc., publishers.




Multidisciplinary teams face numerous challenges as they respond to an outbreak of Ebola virus disease in the remote, forested regions of the Democratic Republic of the Congo. The World Health Organization (WHO) and partners are supporting the country’s Ministry of Health in all aspects of the response, including epidemiological investigation, surveillance, logistics and supplies, communications, and community engagement.

An electronic sepsis alert using a combination of vital signs, risk factors and physician judgment to identify children in a pediatric emergency department with severe sepsis reduced missed diagnoses by 76 percent. The results of the study, along with an accompanying editorial, were published online Friday in Annals of Emergency Medicine ("Improving Recognition of Pediatric Severe Sepsis in the Emergency Department: Contributions of a Vital Sign-Based Electronic Alert and Bedside Clinician Identification" and "Between the Devil and the Deep Blue Sea: Use of Real-Time Tools to Identify Children with Severe Sepsis in the Pediatric Emergency Department").

The world may be closer to knowing why Ebola spreads so easily thanks to a team of researchers from Tulane University and other leading institutions who discovered a new biological activity in a small protein from the deadly virus. The team's findings were recently published in the Journal of Virology.


New advice on which antibiotics to use for common infections and which to preserve for the most serious circumstances is among the additions to the World Health Organization (WHO) model list of essential medicines for 2017. Other additions include medicines for HIV, hepatitis C, tuberculosis and leukemia.

A clinical trial of an experimental vaccine to prevent infection with chikungunya virus is now enrolling healthy adult volunteers at three sites in the United States. The Phase 1/2 trial, which is sponsored by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, is being conducted at several NIAID-funded Vaccine and Treatment Evaluation Units. The candidate vaccine, MV-CHIKV, was developed by Themis Bioscience of Vienna, Austria.
Researchers at Memorial Sloan Kettering Cancer Center in New York have discovered that bacteria living in the gut provide a first line of defense against severe Listeria infections. The study, which will be published June 6 in the Journal of Experimental Medicine, suggests that providing these bacteria in the form of probiotics could protect individuals who are particularly susceptible to Listeria, including pregnant women and cancer patients undergoing chemotherapy.



In healthcare facilities, Clostridium difficile infections spread by transmission of bacterial spores. Appropriate sporicidal disinfectants are needed to prevent development of clusters and outbreaks. In this study by Kenters, et al. (2017), different cleaning/disinfecting wipes and sprays were tested for their efficacy against spores of distinctive C. difficile PCR ribotypes.


One of the primary ways physicians diagnose urinary tract infections is with a test that detects bacteria in urine. A new enhanced test, developed at Loyola University Chicago, detects significantly more bacteria than the standard test, according to a study presented at a meeting of the American Society for Microbiology in New Orleans.
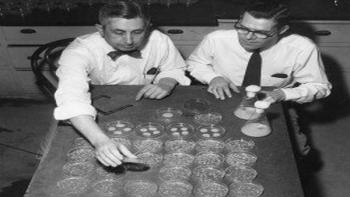
Seventy-three years ago Tuesday, on June 6, 1944, the D-Day invasion of Normandy was bolstered by millions of doses of a precious new substance: penicillin. On the other side of the Atlantic, researchers at the University of Wisconsin–Madison and other institutions had spent the last three years pursuing advances in penicillin production. Though discovered 16 years prior, the world’s first natural antibiotic was expensive and difficult to wring from the mold that makes it. By discovering new strains, isolating more productive mutants, and improving growing methods, UW-Madison biologists helped supply Allied troops with enough penicillin to treat life-threatening infections.

In a new research paper published in the Journal of the American Geriatrics Society, Thomas E. Finucane, MD, of the Johns Hopkins Geriatrics Center at Johns Hopkins in Baltimore, suggests that prescribing antibiotics for urinary tract infections (UTIs) may often be avoided among older adults.

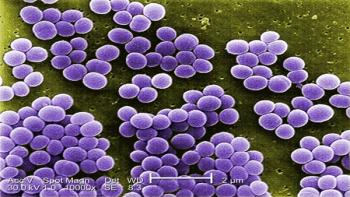
Findings from a study that looked at susceptibility trends of Staphylococcus aureus in U.S. hospital patients showed that key antibiotics used to treat the bacteria became more active over the course of the study, a rare occurrence. Researchers at JMI Laboratories evaluated susceptibility trends of antibiotics from 2009 to 2015 by testing clinical isolates from medical centers across the U.S. The research is presented on June 4th at the ASM Microbe conference in New Orleans.


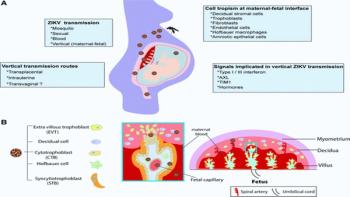
The devastating effects of Zika virus on the brain of the developing fetus during infection in pregnancy have led to intensive research to understand the routes of Zika virus transmission and how the virus travels to and infects the fetus. What researchers have learned about how Zika virus impacts pregnancy and neonatal outcomes and the promise of new therapeutic interventions are presented in a comprehensive review article published in Journal of Interferon & Cytokine Research (JICR) from Mary Ann Liebert, Inc., publishers.

Competing priorities, life-and-death situations and a vast quantity of unknown variables are the hallmarks of the emergency department (ED), and compliance with infection prevention and control (IPC) principles and practices can be challenging. Katherine West, BSN, MSEd, CIC, points to the directive from the Occupational Health and Safety Administration (OSHA) -- CPL 02-02.069 -- that indicates that the delivery of healthcare should not be delayed. "Trauma response is more important than infection control compliance, and even OSHA recognizes that fact," West says. "We have a duty to meet the patient care needs."

With the U.S. healthcare reform mandate for increasing transparency and improved quality, the need for infection prevention and control in long-term care facilities (LTCFs) is becoming more critical than ever before for the more than 3 million Americans receiving geriatric care in U.S. annually. Consider these facts regarding infection in long-term care: • An estimated 1.6 million to 3.8 million infections occur in long-term care facilities each year. • More than 1.5 million people live in 16,000 nursing homes in the United States. Estimates suggest infections could result in as many as 380,000 deaths among those residents each year. • The nursing home population is expected to increase to about 5.3 million people by 2030.