News





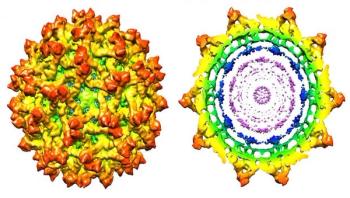
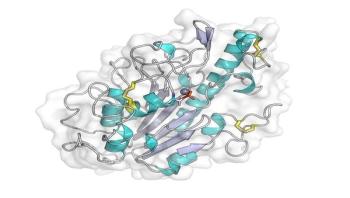
Researchers at Purdue University have determined the high-resolution structure of immature Zika virus, a step toward better understanding how the virus infects host cells and spreads.









2017 promises to present a number of continuing and new challenges for the infection prevention and healthcare epidemiology community. One of the most significant for the field as well as the entire country is a new Presidential Administration. Sara Cosgrove, MD, MS, FSHEA, FIDSA, associate professor of medicine and epidemiology at Johns Hopkins University, and the 2017 president of the Society of Healthcare Epidemiologists of America (SHEA), acknowledges what she characterizes as "an enormous amount of uncertainty" about how a revamped White House and Congress could impact infection prevention and antibiotic stewardship-related issues.

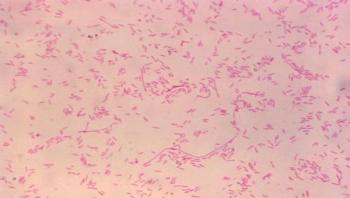
An international research team, led by the University of Bristol, has provided the first clues to understand how the mcr-1 gene protects bacteria from colistin, a last-resort antibiotic used to treat life-threatening bacterial infections that do not respond to other treatment options.

A University of Alberta engineering researcher has developed a new way to treat common surgical masks so they are capable of trapping and killing airborne viruses. His research findings appear in the prestigious journal Scientific Reports, published by Nature Publishing Group.

Scientists have found potential evidence of Ebola virus replication in the lungs of a person recovering from infection, according to new research published in PLOS Pathogens. The findings could aid research into new treatment approaches and better understanding of how the virus is transmitted.




In the short time that it takes to make my favorite meal, shrimp pad Thai (20 minutes), one equally rapid and reliable laboratory test, Procalcitonin (PCT), can quickly inform a licensed healthcare provider that their patient has a bacterial infection, not a viral infection, and halt a fatal outcome (BioMérieux, 2016; Food and Drug Administration, 2012; Lee, 2013; Pantelidou and Giamarellos-Bourboulis, 2015; Schuetz and Mueller, 2016). The untimely identification of antibiotic-resistant bacterial infections is the No. 1 cause of human deaths occurring from sepsis-related events and has increased three-fold over the last decade (World Sepsis Day.org, 2016). Antibiotic stewardship is a necessary fundamental in the battle against antibiotic-resistant infections and should be a priority for all healthcare facility types; antibiotic stewardship is not confined to hospitals (O’Brien and Gould, 2013).



In 2012, the World Health Organization set two public health goals for Gambian sleeping sickness, a parasitic disease spread by the tsetse fly. The first is to eliminate the disease as a public health problem and have fewer than 2000 cases by 2020. And the second goal is to achieve zero transmission around the globe by 2030. Now, by mathematically modeling the impact of different intervention strategies, researchers reporting in PLOS Neglected Tropical Diseases have described how two-pronged approaches, integrating medical intervention and vector control, could substantially speed up the elimination of sleeping sickness in high burden areas of the Democratic Republic of Congo (DRC).