
News















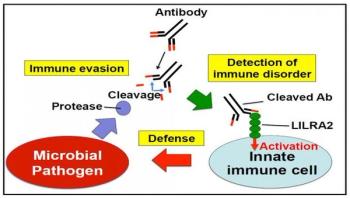
For the first time in the world, a group of researchers discovered a human immune receptor, which detects the invasion of pathogenic microorganisms. They thereby succeeded in identifying a so far unknown host defense mechanism. These results will contribute to future developments in the treatment and prevention of infectious diseases.




In an article published in PLoS Genetics on July 5, scientists from the Institut Pasteur and the Belgian-based Université catholique de Louvain identify for the first time the genetic and metabolic mechanisms underpinning the therapeutic action of a bacteriophage known for its therapeutic potential. Given the worrying rise in bacterial resistance to antibiotics and the difficulties in developing effective new molecules, there has been renewed interest within the scientific community in recent years in phage therapy, which makes use of these bacterial viruses. This discovery will contribute to ongoing efforts to develop this treatment, which has been largely neglected in Western countries.

With the Ebola crisis in the rearview mirror but lurking, cases of C. difficile on the rise, and other known and emerging viruses creeping across the globe, health leaders are focusing greater attention on protecting the people on the front lines of care. The proper removal of personal protective equipment (PPE) – think masks, gloves and gowns – ranks among the most critical of those topics and it’s one infection preventionists should address with physicians, nurses and other healthcare personnel sooner rather than later. The need is pressing. Recall that Ebola infected more than 500 health workers in West Africa in 2014. Meanwhile, other professionals have contracted C. diff and MERS. Experts have not been able to irrefutably link those occurrences to improper PPE removal; however, they have enough experience to posit with authority that poor technique has played a role in at least some of the diagnoses. The reason is simple: Too few healthcare workers take off their PPE in such a way that does not pollute their clothing or skin. To wit, a recent study published by JAMA Internal Medicine showed that 46 percent of doffing simulations engendered some level of contamination.

The reporting of any type of healthcare-associated infection (HAI) is difficult. First, it indicates our patients have experienced a complication. Second, for an acute-care facility, we consistently have a low denominator; therefore any HAI has a significant impact on an infection rate that is publically reportable. This hospital was pleased to report an infection rate of zero for catheter associated urinary tract infections (CAUTIs) for more than two years. Unfortunately, in 2015, three of our patients experienced a CAUTI which dramatically increased the reported infection rate and raised important concerns. Urinary tract infections are the most common type of HAI reported to the National Healthcare Safety Network, with more than 75 percent of those UTIs being catheter associated. The literature tells us that the impact of these infections includes increased length of stay, increased costs, unnecessary antimicrobial use, and is the leading cause of secondary bloodstream infections which results in increased mortality rates. Determining the cause for the increase in infections experienced at this facility and developing strategies to decrease these HAIs became a priority.



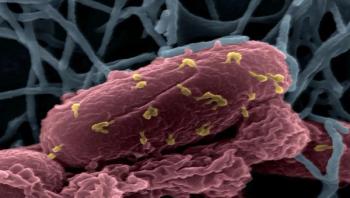
A deadly bacteria that can be picked up by a simple sniff can travel to the brain and spinal cord in just 24 hours, a new Griffith University and Bond University study has found. The pathogenic bacteria Burkholderia pseudomallei, which causes the potentially fatal disease melioidosis, kills 89,000 people around the world each year and is prevalent in northern Australia and southeast Asia.

