Stage May be Set for Next COVID-19 Surge
Beating back infection is a numbers game: viruses against antibodies. If the virus changes its armor so the antibodies cannot attach, it develops an advantage. However, it can also produce viruses which are more efficient at attaching to and invading cells, or simply just produce a lot more viruses, overwhelming the system.
As we are on the beginnings of another COVID-19 surge, many are starting to question whether we can vaccinate our way out of this pandemic. Can we vaccinate our way into herd immunity? Possibly not, because 3 barriers are shedding doubt on accomplishing this goal.
I. Viral Mutations: First, the emergence of the Delta variant (B.1.617.2) has many concerned. We may be entering a period of another major surge in the United States. Initial laboratory studies regarding the efficacy of mRNA vaccines in countering the escape mutations produced by the Delta variant were encouraging. A study by Edara VV, et. al reported a decrease in antibody neutralizing activity for the Delta variant of 3.0% and 3.3% for the Moderna and Pfizer/BioNTech vaccines respectively. Interesting, for the related Kappa variant which is common in India (B.1.617.1), the neutralizing activity of vaccines had almost a seven-fold decrease. A three-fold decrease in protection is well within the efficacy margins for the vaccine, this is good news. Then the reports started emerging out of Israel.
Kevin Kavanagh, MD

The Delta variant comprises more than 90% of the infections in Israel and vaccine efficacy in preventing symptomatic disease has fallen to 64%. mRNA vaccines appear to still be highly effective in preventing deaths and hospitalizations, but data are still out regarding the propensity of those becoming infected to develop long COVID. In Oklahoma, a recent outbreak in a gymnastic gym involved 47 individuals. Seven were vaccinated. 39% of Oklahoma’s population is fully vaccinated, this equates to a 62% vaccine protection rate. All of the sequenced samples were the Delta variant.
One might ask, why are the clinical observations regarding vaccine effectiveness out of line with the laboratory observations? The answer is: Increase in infectivity. The Delta variant spreads about 225% faster than the wild type of virus. Many do not understand that an increase in infectivity cannot only mean the disease spreads easier, but also that it can more easily evade immunity.
The reason is that beating back an infection is largely a numbers game. It is viruses against antibodies. Each side has only so many soldiers. If the virus changes its armor so the antibodies cannot attach, it develops an advantage. However, it can also produce viruses which are more efficient at attaching to and invading cells, or simply just produce a lot more viruses. Both of
Lindsay Cormier, PhD

these latter mechanisms will increase infectivity, but they will also help avoid the body’s immune response. In the case of the Delta variant, it has been found to produce a 1000 times higher viral load than the wild type of virus, suggesting a “potential faster viral replication rate.” A higher viral load will increase the chances of the virus to be able to transmit between hosts, but it also will make the infection harder for the body to combat, since more antibodies are needed to eliminate the infection.The bottom line is that the virus can evade immunity by at least 3 mechanisms:
- Making it harder for antibodies to attach, thus, requiring more antibodies to eliminate an infection.
- Increasing the attachment efficiency of the virus such that less viruses are required to perpetuate an infection.
- By producing more viruses such that more antibodies are required to eliminate the invaders. In other words, it overwhelms the immune system.
II. Animal Reservoirs: Second, we have stated many times before that the coronavirus does not care about politics, it is out to win and will infect everyone equally, regardless of their political persuasion. The same can be true for infections with other species. SARS-CoV-2 does not care if you are a human, cat, dog or bear. It will infect and then mutate to optimize its spread between similar hosts.
An article published in the Proceedings of the National Academy of Sciences should serve as a warning regarding “the spillover of SARS-CoV-2 from humans to other susceptible animals.” Evaluating the similarities of the ACE2 receptor, the researchers found that mammals had a medium or high affinity for receptor binding and catarrhine primates were in a very high category.
SARS-CoV-2 has been reported to commonly infect domesticated dogs and cats. One report found studied 48 cats and 54 dogs from 77 households with SARS-CoV-2 positive owners. Sixty-seven percent (32) of the cats tested positive, 41% (13) cats had symptoms characterized by a runny nose and difficulty breathing. In three cases, the illness was severe. Forty-three percent (23/54) of the dogs tested positive for SARS-CoV-2. Forty-eight percent (11) of infected dogs had symptoms, mainly lack of energy and appetite, but some developed a cough and diarrhea. All of the dogs had mild infections.
Zoo animals such as large cats and gorillas have become infected with COVID. The Oakland Zoo has begun an experimental COVID vaccine on tigers, bears, lions and ferrets. Additional zoos, including the San Diego Zoo in California, the Columbus Zoo in Ohio, the Louisville Zoo in Kentucky, the John Ball in Grand Rapids, Michigan, and the North Carolina Zoo in Asheboro are planning vaccinations in the near future. Birds can also become infected with coronaviruses, but to date infections with SARS-CoV-2 have not yet been reported. However, the proclivity of SARS-CoV-2 to mutate and jump between animal species makes this a future possibility
III. Vaccine Hesitancy: There have been multiple iterations of SARS-CoV-2 in a little over a year. The U.S. population is exceedingly vaccine hesitant with only 48% of individuals fully vaccinated. Vaccines will also slow the spread of variants and help protect our population from severe disease. And there are other variants waiting their turn to infect our society, the Delta Plus (AV.2), Eta (B.1.525), and Lambda (C.37). All of which is very worrisome. These variants have already landed on our shores but according to outbreak.info, they have not yet begun to spread. This may indicate that the Delta variant is outcompeting these variants and preventing them from becoming V strains.
Slow the Spread
Animal reservoirs may well serve as a source of viral outbreaks in the future along with potentially endangering food supplies. However, we are fast developing and implementing a comprehensive program to vaccinate our animals. Unfortunately, we appear to be much less willing and able to do this for homo sapiens.
The bottom line, we need to learn to live with this virus. It is not going to go away. The first steps we must take is to accept this pandemic, embrace public health strategies and get vaccinated to slow down the spread and mutations of this virus.
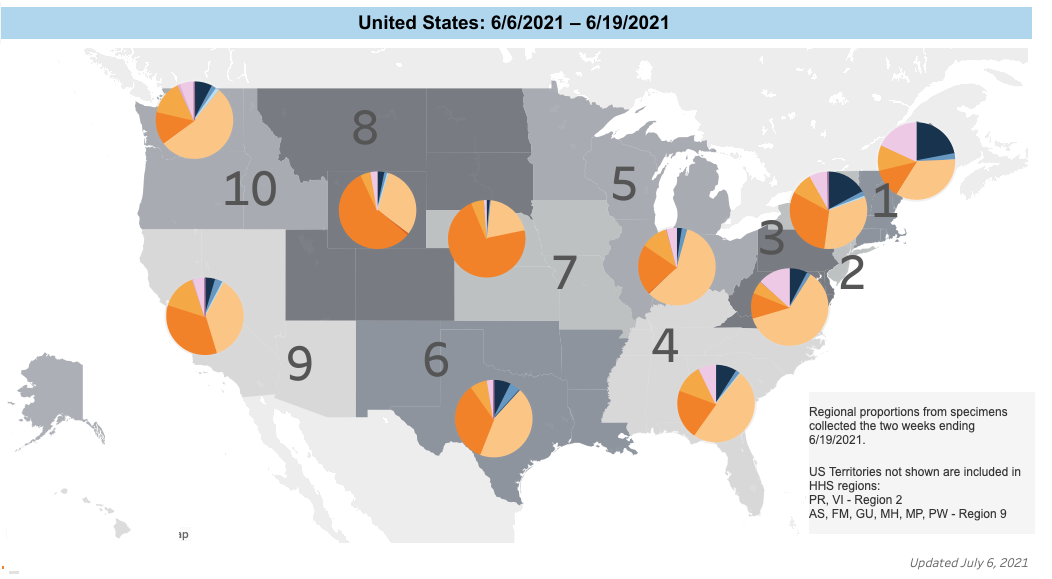
Source: Centers for Disease Control and Prevention
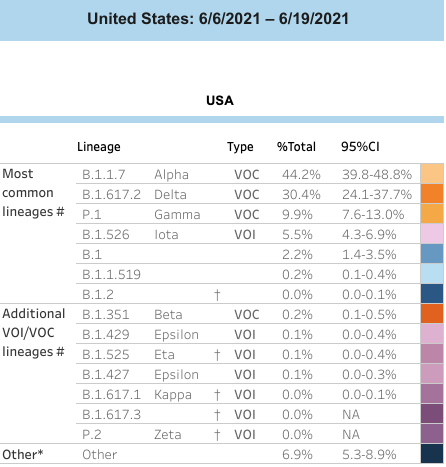
Source: Centers for Disease Control and Prevention
Beyond the Surface: Rethinking Environmental Hygiene Validation at Exchange25
June 30th 2025Environmental hygiene is about more than just shiny surfaces. At Exchange25, infection prevention experts urged the field to look deeper, rethink blame, and validate cleaning efforts across the entire care environment, not just EVS tasks.
A Controversial Reboot: New Vaccine Panel Faces Scrutiny, Support, and Sharp Divides
June 26th 2025As the newly appointed Advisory Committee on Immunization Practices (ACIP) met for the first time under sweeping changes by HHS Secretary Robert F. Kennedy Jr, the national spotlight turned to the panel’s legitimacy, vaccine guidance, and whether science or ideology would steer public health policy in a polarized era.
Getting Down and Dirty With PPE: Presentations at HSPA by Jill Holdsworth and Katie Belski
June 26th 2025In the heart of the hospital, decontamination technicians tackle one of health care’s dirtiest—and most vital—jobs. At HSPA 2025, 6 packed workshops led by experts Jill Holdsworth and Katie Belski spotlighted the crucial, often-overlooked art of PPE removal. The message was clear: proper doffing saves lives, starting with your own.