
News





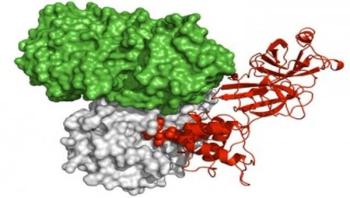
The first three-dimensional image capturing a critical malaria 'conductor' protein could lead to the development of a new class of antimalarial drugs. Researchers from Melbourne's Walter and Eliza Hall Institute developed WEHI-842, a drug that blocks the malaria parasite protein plasmepsin V, killing the parasite. The discovery is a new step toward developing much needed new drugs for treating and preventing malaria.
This week at the American Crystallographic Association (ACA) 2015 meeting in Philadelphia, researchers from the National Cancer Institute will present three newly determined crystal structures, which collectively provide a starting point for structure-based drug design efforts to combat MERS. The work will be presented by George Lountos, a scientist in the lab of primary investigator David Waugh.


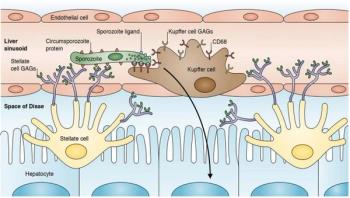
Scientists uncover a port of liver entry for malaria parasites in a report published in the Journal of Experimental Medicine. If these results hold up in humans, drugs that target this entry protein might help prevent the spread of disease.
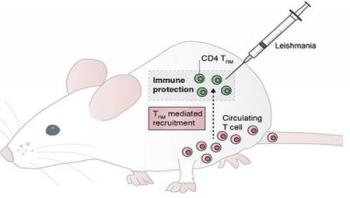
Immune cells that hang around after parasitic skin infection help ward off secondary attack, according to a study in the Journal of Experimental Medicine. These skin squatters may prove to be the key to successful anti-parasite vaccines.




Surgical site infections (SSI) continue to remain a national healthcare issue, raising costs due to prolonged hospitalization, additional diagnostic tests, treatment, and sometimes additional surgery. In fact, research suggests that SSIs can extend hospitals stays by seven to 10 days and cost $27,402 per incident, accounting for up to $10 billion annually in healthcare spending. That’s why Medline is working in partnership with the Joint Commission Center for Transforming Healthcare and Cleveland Clinic to share the latest SSI findings with healthcare leaders and medical device and clinical solution developers. The goal: uncover some of today’s real problems and barriers to spark serious dialogue and solutions.









In Sierra Leone, the Ebola outbreak has affected all aspects of healthcare. Exact numbers are yet to be confirmed but it is clear that many children have missed out on routine vaccination services and birth registration during the outbreak. To counter this, mass immunization campaigns are being held to enable children to catch up. In June this year, an integrated measles and polio campaign was conducted reaching 97 percent of children under the age of 5.



A new discovery by Michigan State University (MSU) scientists suggests that a common medication used to treat glaucoma could also be used to treat tuberculosis, even the drug-resistant kind. Robert Abramovitch, an MSU microbiologist, along with graduate student Benjamin Johnson who helped lead the study, have discovered that ethoxzolamide, a sulfa-based compound found in many prescription glaucoma drugs, actually turns off the bacterium's ability to invade the immune system.

Controlling mosquitoes that carry human diseases is a global health challenge as their ability to resist insecticides now threatens efforts to prevent epidemics. Scientists from the CNRS, IRD, Université Claude Bernard Lyon 1, Université Joseph Fourier in Grenoble and Institut Pasteur in French Guiana have identified new genetic markers for mosquito resistance to insecticides, which could improve its detection in the field. This work was published in Genome Research on July 23, 2015.