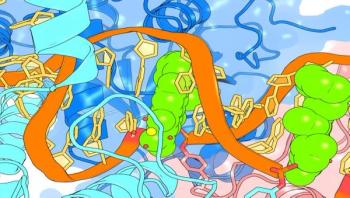
Virulent strains of bacteria are ones that produce "virulence factors," small molecules and proteins that convert a benign bacterium into a pathogen. They make the difference between E. coli that are helpful members of our gut microbiome and the E. coli O157:H7 responsible for the Jack-in-the-Box outbreak. Virulence factors allow bacteria to evade the human immune system, to infect tissues and cells and to establish a foothold within the body. Without them, bacteria would be rapidly cleared by the immune system and unable to establish an infection.Tim Wencewicz, PhD, assistant professor of chemistry in Arts & Sciences at Washington University in St. Louis, thinks we should be looking for agents that block virulence factors rather than continuing to search for ones to kill bacteria outright. In his vision, antivirulence antibiotics would replace failing bactericidal ones.