
News



A growing risk of outbreaks of measles, pertussis, and other vaccine-preventable diseases in countries affected by Ebola must be countered by urgent scaling up of routine immunization activities, according to the World Health Organization (WHO).


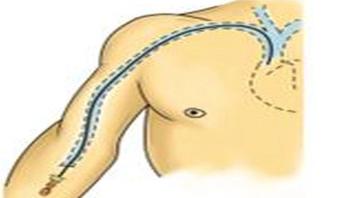
Every day, patients around the country get IV devices placed in their arms, to make it easier to receive medicines or have blood drawn over the course of days or weeks. But these PICC lines also raise the risk of potentially dangerous blood clots. Now, a University of Michigan Medical School team has shown how serious that clot risk really is for hospitalized patients, and what factors put patients at highest risk.



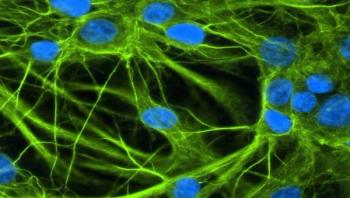
Wireless sensors recording human interactions explain the transmission of MRSA in hospitals, according to research by Thomas Obadia and colleagues. The study, published this week in PLOS Computational Biology, reveals that close proximity interactions between patients and healthcare workers in Berck-sur-Mer hospital, France, acted as pathways for the transmission of Staphylococcus aureus strains.


Dr. Pierre Formenty has spent the past 20 years investigating communicable disease outbreaks, including many Ebola outbreaks. In mid-March 2014, while in Kinshasa, training healthcare workers to safely take and dispatch blood samples that may contain ‘dangerous pathogens’ such as Ebola virus, he began receiving emails that got him worried.





A new analysis of a medieval cesspit in the Christian quarter of the old city of Jerusalem has revealed the presence of a number of ancient parasite eggs, providing a window into the nature and spread of infectious diseases in the Middle East during the 15th century. Researchers found evidence of six species of intestinal parasites in the over 500-year-old latrine. These included large quantities of roundworm and whipworm, both spread by fecal contamination of food and thought to be endemic to the region dating back to human evolution out of Africa.

When Mary Mwape, a midwife, delivers babies at Lubwe Mission Hospital in Luapula Province of Zambia, there’s often no water to wash her hands or clean the newborn. Yet mothers from all over the region are referred to the hospital for delivery and related healthcare activities.












Engineers at the University of California, Berkeley, are developing a new type of bandage that does far more than stanch the bleeding from a paper cut or scraped knee. Thanks to advances in flexible electronics, the researchers, in collaboration with colleagues at UC San Francisco, have created a new "smart bandage" that uses electrical currents to detect early tissue damage from pressure ulcers, or bedsores, before they can be seen by human eyes - and while recovery is still possible.