
After an Expo like no other, Dennis looks forward to the 70th year of advocacy for perioperative nurses.

After an Expo like no other, Dennis looks forward to the 70th year of advocacy for perioperative nurses.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending April 8.

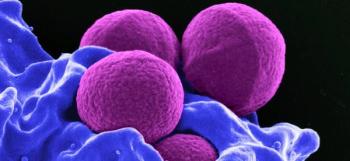
From 2014 to 2021, continued FDA reports have shown multidrug-resistant bacteria contaminating 6 types of endoscopes have had fatal consequences.

The letter comes after a year of reprocessing validation testing and a voluntary medical device recall.

Rethinking the application of air disinfection in the era of COVID-19.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending March 25.

The technology allows the drape to be used without harming fragile or sensitive skin.

Summary: Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending March 18.

ANSI/AAMI’s update on endoscope processing is backed by rigorous scientific evidence.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending March 11.

A letter has been sent to more than 4500 veterans stating that reusable instruments used in medical procedures may not have been sterilized properly at a Georgia hospital.

Proper ventilation can greatly reduce the environmental strain on operating rooms. However, there’s no one-size-fits all solution.

The successful combination of products and the adoption and application of science-based practices will help the sterile processing profession rise above challenges to protecting frontline technicians.

“[Personal protective equipment] was splashed during most activities and did not prevent skin exposure even when properly donned and doffed,” the study states.

La’Titia Houston MPH, BSN, RN, CIC: “We work not only with the bedside nurses and the sterile processors, but even with our clinicians, our physicians. They want a timeout before the procedure is even performed because they want to ensure that the scope did pass during the high-level disinfection procedure.”

Testing of the infant of the COVID-19–positive mother requires 2 negative COVID-19 tests 2 days apart. This time delay adds to the challenge of ensuring available isolation beds.
The makeup and application of surgical drapes hasn’t significantly changed in 50 years, a study states. Time for a new look?

Many infection preventionists trust that everyone working in the operating room knows what they are doing and many times shy away from going into the OR. That's a mistake.

Linda Spaulding RN, BC, CIC: “It only takes you saying something a couple times that the OR knows is absolutely absurd and incorrect, and it’s going to ruin the relationship for a long time. Infection preventionists really need to take the responsibility of learning.”

Tanya Lewis, CRCST: “I just think that infection preventionists and sterile processors should always work as a team. It should always be a team effort. It’s not them or us. It’s not sterile processing. It’s not infection prevention, but it’s us as a team. And that’s the way we’re going to keep our patients safe.”
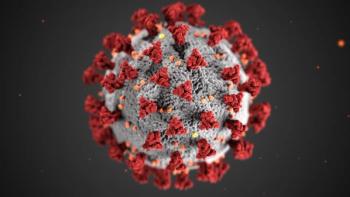
Though tough months lie ahead for infection preventionists and other healthcare professionals, hope remains that at some point in 2021 things will begin to settle down. In the end, it comes down to a simple formula: We win, COVID-19 loses.

Linda K. Groah, MSN, RN, CNOR, NEA-BC, FAAN: “Historically, we have not always had the best relationship. There’s been some competition between infection preventionists and OR managers or directors. The operating room has been that secret area behind the double doors.”
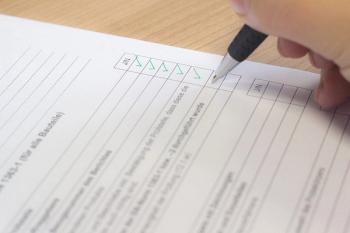
New infection preventionists can use this checklist to perform IP rounds in the surgical suite, decontamination areas, and sterile processing area.

Franklin Dexter, MD: “I would recommend to those people working in different surgical suites to recognize that within an operating room, you shouldn’t assume that stepping away from the patient would put you in reduce risk. You should think about what the airflow is in the operating room.”
