
News


An international team of researchers from the University of Rome Tor Vergata and the University of Montreal has reported, in a paper published this week in Nature Communications, the design and synthesis of a nanoscale molecular slingshot made of DNA that is 20,000 times smaller than a human hair. This molecular slingshot could “shoot” and deliver drugs at precise locations in the human body once triggered by specific disease markers.



Several years following a widely publicized series of outbreaks related to contaminated and improperly reprocessed duodenoscopes, re-searchers are reporting that current techniques used to clean endoscopes for reuse are not consistently effective. However, some experts say that slow progress is underway.

Some central service (CS) professionals find comfort in knowing their chosen discipline provides them with a secure “job.” The fact is, though, that the dynamic, fast-paced and ever-evolving realm of CS/sterile processing delivers a challenging, yet rewarding career filled with rich opportunities for growth and advancement.

As an infection prevention consultant with 25-plus years of experience, I frequently audited healthcare facilities regarding proper reprocessing of their surgical, dental and/or endoscopic equipment. With each audit, I found healthcare professionals who had a strong desire to learn and adhere to best practices. This is important, as best practices should be adhered to in any profession because they reflect the values of that profession. In healthcare, adherence to sterilization and disinfection best practices ensures patient safety, as one of our greatest threats is healthcare-associated infections (HAIs). That said, I sometimes found it difficult to get everyone on board with compliance with national standards and guidelines, such as the Association for the Advancement of Medical Instrumentation (AAMI), the Association of periOperative Registered Nurses (AORN) and/or the Society of Gastroenterology Nurses and Associates (SGNA). In recent years, my efforts were reinforced with help from two very important organizations, the Joint Commission and the Centers for Disease Control and Prevention (CDC).

It has been more than 10 years since The New England Journal of Medicine published the Keystone project’s ground breaking work on reducing ICU CLABSIs using a central line insertion bundle. Since that time, this has become the absolute standard throughout healthcare settings in the United States. When it comes to completing the central line insertions checklist, many of us only accept “yes” and “yes with prompting” as possible responses. Our accrediting agencies expect this as a standard of practice.


Researchers at the University of Notre Dame have discovered a way to make influenza visible to the naked eye, according to a new study in the Journal of the American Chemical Society. By engineering dye molecules to target a specific enzyme of the virus, the team was able to develop a test kit that emitted fluorescent light when illuminated with a hand-held lamp or blue laser pointer.



To combat potential outbreaks of the Zika virus, some countries have considered using pesticides so strong that they are banned elsewhere. But if you could quickly determine that mosquitoes were not carrying the Zika virus, the use of harmful pesticides could be avoided, as well as the cost of widespread spraying. That’s the premise behind a new study published May 3 in Science Translational Medicine, authored by assistant professor Joel Rovnak, graduate student Nunya Chotiwan, and research associate Connie Brewster in Colorado State University’s Department of Microbiology, Immunology and Pathology.




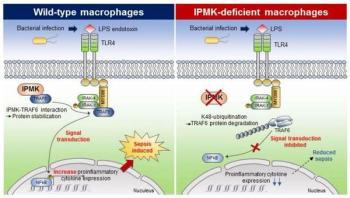
Professor Seyun Kim's team from Korea Advanced Institute of Science and Technology (KAIST) reported the mechanism by which cellular signaling transduction network is exquisitely controlled in mediating innate immune response such as sepsis by the enzyme IPMK (Inositol polyphosphate multikinase) essential for inositol biosynthesis metabolism.








Nonalcoholic fatty liver disease (NAFLD) - a condition that can lead to liver cirrhosis and cancer - isn’t typically detected until it’s well advanced. Even then, diagnosis requires an invasive liver biopsy. To detect NAFLD earlier and more easily, researchers in the NAFLD Research Center at University of California San Diego School of Medicine, Human Longevity, Inc. and the J. Craig Venter Institute report that the unique microbial makeup of a patient’s stool sample - or gut microbiome - can be used to predict advanced NAFLD with 88 to 94 percent accuracy.
