Coronavirus disease 2019 (COVID-19) has made hand hygiene all the rage. That’s too bad. Because hand hygiene doesn’t only help to slow the spread of COVID-19, but a slew of other dirty bugs, as well.
Coronavirus disease 2019 (COVID-19) has made hand hygiene all the rage. That’s too bad. Because hand hygiene doesn’t only help to slow the spread of COVID-19, but a slew of other dirty bugs, as well.

Charles P. Gerba, PhD: “Unfortunately, standard procedures for testing and registration by regulatory agencies of CADs (continuously active sanitizers or disinfectants) as disinfectants useful in preventing exposure to disease causing microorganism transmission has only taken place in recent years.”

With inadequate disinfection practices, healthcare workers are much more likely to acquire pathogens on their hands after touching these surfaces, potentially passing them on to patients.
As the pandemic seems not to abate, patients will start to present to the hospital after delaying crucial primary and preventive care visits, meaning sicker non–COVID-19 infected patients, with the potential for increased CLABSI and CAUTI rates.

Before 2000, I was uncommon in the United States. I’ve become much more common since, and though health experts don’t know just how many people I infect each year, they can say with certainty that I am a major cause of infections in healthcare settings.

After decades of reluctance to implement a national reporting system, when COVID-19 came along we witnessed almost overnight the formulation of case definitions and comprehensive national reporting from all healthcare facilities.

The common method used to determine IP staffing-using a ratio of IPs to the number of beds or the number of patients-might not be the best way of determining just how many IPs an institution needs.

IIn the latest Morbidity and Mortality Weekly Report from the Centers for Disease Control and Prevention (CDC), researchers discuss SARS-CoV-2 in two domestic cats.

Infection preventionists (IPs) are stretched to the limit with both reporting and patient responsibilities with an unwillingness of facilities to prioritize infectious disease prevention in their operating budgets.

Sharon Ward-Fore: "Rather than reusing gowns, consider bundling patient care activities to conserve gowns. Donning a gown that has already been used can be tricky, and a source of contamination to the user."

Small clusters of environmental transmission in gyms and other workout settings can tell us about potential risky environments in healthcare. Outpatient physical therapy for one.

Ideally, link nurses increase awareness of infection control issues and motivate colleagues to improve in that regard, keeping patients and themselves safer by limiting the spread of HAIs.

Infectoin preventionists's can bring their perspective and strengths to the antimicrobial stewardship (AMS) program and offer ways to bring the work to the bedside and engage the partnerships that already exist to make AMS programs successful.

Although all patients require vigilant infection prevention measures and the goal should always be zero infections, the stakes are sometimes higher in the NICU, as infections there have higher potential for death.

Xenon lamps produce pulsed flashes of germicidal UV light at wavelengths from 200-315 nm, killing microbes on environmental surfaces.

As the threat from COVID-19 increases, so must the readiness of infection preventionists to respond.

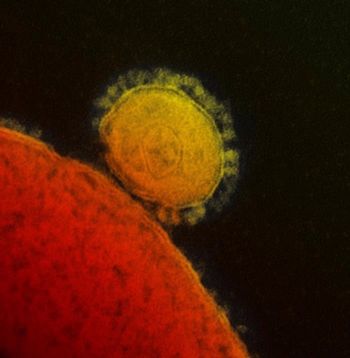
The CDC is more pessimistic than the WHO about containing the novel coronavirus COVID-19.

Christina Tan, MD, MPH, state epidemiologist and assistant commissioner with the New Jersey Department of Health, discusses the current coronavirus outbreak and how infection prevention efforts can help curb its spread.

Infection control specialists need to know how to successfully design and implement an effective infection prevention program.


“These estimates are reassuring,” says Brendan Flannery, PhD, the CDC’s investigator for the US Flu Vaccine Effectiveness Network.

Hospital administrators and infection preventionists have to contend with diversity among C. diff isolates.
Health officials say that this is a particularly bad year for an extended influenza season since flu symptoms and some of the symptoms of the novel coronavirus, COVID-19, are the same (fever, cough, shortness of breath).

The agency uses an emergency use authorization to allow distribution of the diagnostic kits.