
HAIs
Latest News



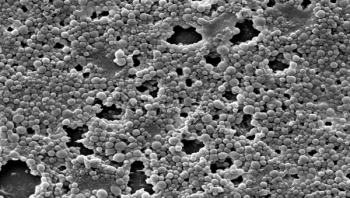
Biofilms, or colonies of bacteria growing on surfaces and medical devices, can inflict intractable or recurring disease. During colonization, biofilms develop characteristics and behaviors more dangerous and powerful than those of planktonic (singleton) bacteria. In fact, these insidious microscopic collectives could be regarded as biological case studies in “strength in numbers” as they unify against external assault, resisting the host immune response as well as antimicrobials, and exact their high human and fiscal costs. Puzzlingly, although biofilms are a ubiquitous, well documented cause of infection, they receive only a modicum of the attention they clearly merit.

Healthcare-acquired infections (HAIs) are among the leading causes of patient disability and mortality as well as financial loss for health care institutions with hundreds of millions of patients affected and the United States losing approximately $6.5 billion annually. Despite efforts to solve the HAI problem, 3.5 percent to 12 percent of patients are affected each year. HAI are often due to factors such as insufficient application of hygienic practices and hospital protocols.(1)

This digital issue explores disease caused by emerging infectious threats as well as hospital pathogens, and the interventions – such as hand hygiene, contact precautions and environmental cleaning – that can be used to control and prevent infection transmission.

Infection preventionists (IPs) continue to be consumed with keeping up with evolving infection prevention imperatives, according to an online survey conducted by ICT that asked respondents what they believed were the most important issues facing the entire infection prevention and hospital epidemiology community in 2016. Other top issues on their minds for the new year included addressing antibiotic/antimicrobial resistance, advancing quality improvement and patient safety, addressing emerging pathogens and infectious diseases, and evolving the evidence base to answer unresolved issues.


As healthcare professionals we often wonder how much difference we truly make in the lives of our patients. I often wonder if I am doing everything that I possibly can to create a safe environment for every person around me - not just patients but my team as well. Maybe you are a nurse or tech who has wondered the same. Having worked in healthcare for the last nine years and endoscopy for the last four, I have met a variety of people each with their own story to tell. There are certainly moments that bring to light just how much impact we truly have in someone’s life. Errors often occur due to a lack of education or what I would refer to as follow-the-leader. Someone performs a task incorrectly and it continues until someone questions the process. That is where we come in. I want to encourage all of you to take that step forward and be the advocate that our patients so desperately need. Let me explain why I am so passionate about infection control and what we can do to continue creating a safer environment for all of our patients.
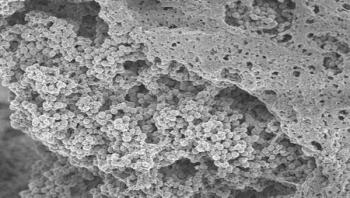
Biofilms frequently coat the surfaces of catheters, and of various medical implants and prostheses, where they can cause life-threatening infections. New research at the Sahlgrenska Academy show that coating implants with a certain "activator" can prevent Staphylococcus aureus, the leading cause of hospital-acquired infections, from forming biofilms.








One weapon in the armament against surgical site infections (SSIs) is the American College of Surgeons' National Surgical Quality Improvement Program (NSQIP), an essential tool to helping hospitals reduce the rate of SSIs and other complications that arise during and after patient procedures, says Clifford Ko, MD, MS, MSHS, FACS, director of the Division of Research and Optimal Patient Care at the American College of Surgeons (ACS). Ko will deliver the keynote address, “Achieving Quality Improvement in Patient Care,” at the OR Manager conference to be held Oct. 7-9, 2015 in Nashville, Tenn.






