
Barbara Smith, RN, BSN, MPA, CIC: “I think that we need to do a little bit more with the public in terms of antibiotic use in the community. So that they’re not at risk for C. diff for whatever reason later in their life.”

Barbara Smith, RN, BSN, MPA, CIC: “I think that we need to do a little bit more with the public in terms of antibiotic use in the community. So that they’re not at risk for C. diff for whatever reason later in their life.”

The rates of Clostridioides difficile remained about the same in March, April, May of 2020 as they were during the same 3 months in 2019, according to the study.

An integrated air management system requires proper engineering and not a pile-up approach of unproven products. One concern is that decision makers will fall into the nearsighted trap of selecting piecemeal products that require frequent maintenance.

At the intersection of surgery and infection prevention resides a sometimes-neglected opportunity to further minimize infection risk by modernizing choices and innovation.

Jody Feigel, RN, MSN: “A few years ago, nobody wanted to hear from infection prevention. Now, everybody wants to hear from infection prevention.”

One of the reasons that S aureus and C diff present such a disinfection challenge is that they are encased in a biofilms such as yeast, protozoa, bacteria, fungi, and algae.

Successful onboarding of candidates requires an orientation that includes all aspects of the position. What are the responsibilities of an IP? Their main function is to identify and mitigate infection risks.

The increasing threat of antimicrobial resistance, exacerbated by the pandemic, underscores the importance of the infection preventionist as an active member of the antimicrobial stewardship program.

Ann Scheck McAlearney, ScD, MS: “Infection preventionists … can provide managers with the guidance provided by this type of research, as well as the data to support infection prevention efforts….”

An actively engaged hospital management team can make the difference between success or failure when it comes to managing health care-acquired infections, a study states.

Hospital employees performed hand hygiene under the gaze of infection preventionists, and the study data were gathered during the COVID-19 pandemic.

Investigators University of Michigan-Flint, School of Nursing noted that the Cooper Tool and the Stone criteria are similar but use different methods to arrive at a UTI diagnosis.
Meri Pearson, MPH, CIC: “Infection preventionists still need to do those active audits to make sure that they’re actually seeing what’s happening at the bedside.”

The number of syphilis cases in 2000 raised hopes that it could be eradicated, but since 2015 cases have risen 74%.

The lessons infection preventionists at the University of Mississippi Medical Center learned from an outbreak of respiratory illness at the facility’s NICU in 2019, were later used to help deal with the COVID-19 pandemic.
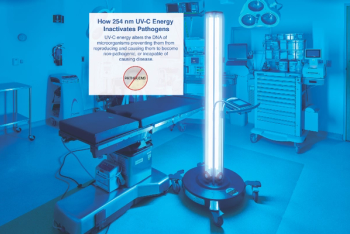
Ultraviolet light should be used in concert with traditional cleaning and disinfection procedures utilized by environmental services teams, study’s author maintains.

The infection prevention and business intelligence teams at Piedmont Healthcare put their heads together to streamline the process of tracking health care-acquired infections.

Emilie Bédard, PhD: “We worked in collaboration with infection prevention, environmental services…. We had a multi-disciplinary team to make sure that we would look at all aspects of this approach.”

The multidisciplinary team included NICU nurses, physicians, nurse practitioners and, perhaps most important of all, environmental services personnel. “We met with the environmental services staff, and we explained to them that this is a critical situation in the neonatal ICU. And this cannot spread more.”

The study comes at a time when—despite all the attention and health care resources being thrown at COVID-19—medical experts have begun to turn a wary eye toward bacteriological pathogens.

When outbreaks have been reported in hospitals that are using universal masking, unmasked exposure to other health care workers is often the cause. Transmissions have been traced to break rooms and cafeterias.
Priya Nori, MD: “The immediate thing that the health care industry has to grapple with, even as COVID hopefully starts to settle down after the mass vaccination campaign … [will be] superbugs.”

Evidence shows that bacteria on floors can be resuspended into the air with a potential of inhalation, swallowing, or contamination of surfaces and hands.

Arjun Srinivasan, MD: “There’s a lot of potential for synergy between the infection prevention program and the antibiotic stewardship program.”

Investigators propose that their simulation models can be used in educating nurses and other health care professionals about how best to maintain good hand hygiene, and also where best to put alcohol-based hand disinfectants.