
Rethinking the application of air disinfection in the era of COVID-19.

Rethinking the application of air disinfection in the era of COVID-19.

IPs can provide valuable input on construction projects, water safety, and ventilation.

The technology allows the drape to be used without harming fragile or sensitive skin.

The system gives infection preventionists another tool to combat the pathogen despite implementation challenges.

Summary: Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending March 18.

A public/private enterprise taps into the entrepreneurial urge that will hopefully help the United States avoid the disastrous shortages of personal protective equipment that deviled the health care system in the first months of the COVID-19 pandemic.

The electrostatic sprayer method kills nearly 100% of pathogens. It also kills the COVID-19 virus. But is that overkill?

La’Titia Houston MPH, BSN, RN, CIC: “We work not only with the bedside nurses and the sterile processors, but even with our clinicians, our physicians. They want a timeout before the procedure is even performed because they want to ensure that the scope did pass during the high-level disinfection procedure.”

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending November 19.

As part of infection prevention against COVID-19, schools spent millions of federal dollars trying to upgrade ventilation systems. That money has been ill-spent, warn some experts.

What does the post-COVID-19 future look like for infection preventonists? Great strides in infection prevention have been made because of the COVID-19 response, but look for them to be modified moving forward.

Vetting new technology and products is a complicated endeavor that takes hours if not weeks before a decision can be made as to whether to bring products into a health care facility. The COVID-19 pandemic did not give health care the luxury of time.

An integrated air management system requires proper engineering and not a pile-up approach of unproven products. One concern is that decision makers will fall into the nearsighted trap of selecting piecemeal products that require frequent maintenance.

Some fear that hospitals will become “Robots R Us” environments, but that is unlikely. Chatbots, although useful, are poor stand-ins for in-depth, in-person conversation with a health care provider. And if COVID-19 did anything, it put a million faces to the tragedy of what it’s like to die without human contact.

Ultraviolet-C light makes benzalkonium chloride, which is found in many disinfectants, safer to use.

COVID-19 helped to speed up adoption of telehealth. When it comes to telehealth platforms, though, there is no such thing as a one-size-fits-all approach.

The shape and material composition of the N95 respirators varied widely from manufacturer to manufacturer, which can result in variations in the efficacy of a particular method from one product to the next.
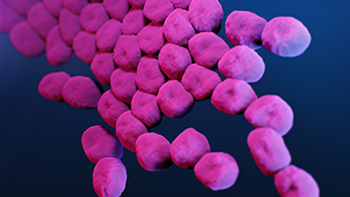
Investigators wanted to see how their method would fare against Acinetobacter baumannii and methicillin-resistant Staphylococcus aureus, and results were promising.

Hand hygiene is always important, but during this pandemic it’s crucial to preventing transmission. Now technology is making it possible for hospitals not only to monitor compliance, but also potential viral exposure.
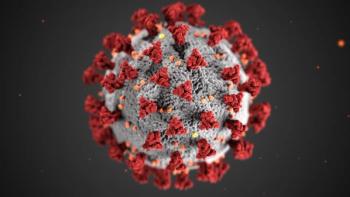
Though tough months lie ahead for infection preventionists and other healthcare professionals, hope remains that at some point in 2021 things will begin to settle down. In the end, it comes down to a simple formula: We win, COVID-19 loses.

Officials at the Children’s Hospital of Philadelphia have the ability to convert several floors into airborne infection isolation rooms (AII), or more commonly termed negative pressure rooms, with the flip of a switch.

W. Frank Peacock, MD, FACEP, FACC, FESC: “When I intubate somebody, I need to know where the tube is, and I need to know now—like within 10 seconds. You can’t tell with anything else. Nothing is as fast as the stethoscope. I can get an X-ray, but I’ve got to wait for the X-ray while you hold your breath.”

Investigators claim that their device can decontaminate N95s and surgical masks in the time it would take an infection preventionist to wash her hands.

Investigators found that a prompt on a disinfection tracking system led to an increase rate of the disinfection of computers on wheels at a veterans’ hospital in Texas.

Maine health officials relied on an automated system to provide contact tracing for COVID-19 to a relatively sparse and spread out population. It worked.