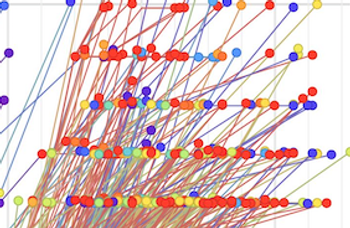
Researchers from China recommend disinfecting the air, alongside, sanitizing surfaces, to reduce exposures and transmission.
Researchers from China recommend disinfecting the air, alongside, sanitizing surfaces, to reduce exposures and transmission.

By their nature, challenge trials have to be performed in young healthy individuals. SARS-CoV-2 is most lethal in the elderly and those with co-morbidities. Thus, an effective vaccine may be found for the young, but not in the elderly with an aging immune system.

Monica Gandhi MD, MPH: “We will get to the end of this [COVID-19]. We will get to a combination of vaccine and natural infection, enough people getting herd immunity that this will stop. This will stop and we will get back to normal.”

The education of IPs has become a topic of interest since the onset of coronavirus disease 2019 (COVID-19). The novel coronavirus highlighted that there perhaps are not enough IPs, and that’s especially true since their knowledge is being sought by schools, businesses and other non-healthcare settings.

Where can we find data on whether or not water vapor is necessary for humans residing in buildings? One great place for such research is the hospital. There is a tremendous amount of data that is collected from one type of hospital building occupant—the patient.

Investigators say that a corrections officer in a Vermont prison had had “multiple brief encounters” with whom the study defines as 6 incarcerated or detained persons (IDPs) who had COVID-19 but did not know it yet.

It’s no longer just a matter of case counts and hospitalizations due to COVID-19, but it’s what we’re seeing in terms of the demographic groups being affected and associative complications.
Study: “There was no difference in the outcome in COVID-19 patients co-infected with influenza compared to non co-infected patients, however, a larger sample of cases will be needed for further assessment of these outcomes.”

CAUTI rates were 83% higher and CLABSI rates were 65% higher in the COVID-19 units compared to the non-COVID-19 units.

There are 4 “moments” involved as a healthcare professional at a long-term care facility (LTCF) weighs whether to prescribe an antibiotic to a patient or resident.

A letter signed by 80 researchers says the concept put forth by the Great Barrington Declaration is “a dangerous fallacy.”
Great Barrington Declaration: “Schools and universities should be open for in-person teaching. Extracurricular activities, such as sports, should be resumed. Young low-risk adults should work normally, rather than from home. Restaurants and other businesses should open.”

Investigators note that during the coronavirus disease 2019 (COVID-19) pandemic, there have been discussions about the role of social distancing in ORs during tracheal intubation and/or extubation, and other aerosol generating procedures.

It can be helpful for infection preventionists to still provide quick COVID-19 rounds in units and high-risk areas like emergency departments and urgent care clinics. These can be as simple as 30-minute reviews of personal protective equipment, isolation precautions, and communication pathways.

Mary Jean Ricci MSN, RNBC: “In most facilities, the infection preventionist is the person doing contact tracing, is assisting the students should there be an exposure, is assisting with providing education on site or real-time education with the students should they see the students take off their PPE.”
For infection preventionists and frontline healthcare workers, the Great Barrington Declaration places their lives and livelihood at risk. A field hospital has been activated in Wisconsin and the state is at risk of running out of hospital beds and trained staff.

Christopher Blank, CIC, MPH, an infection preventionist with BJC Healthcare, sits down with Infection Control Today® to discuss the benefits of making employment for healthcare workers contingent on getting the flu vaccination.
Kevin Kavanagh, MD: “Many of the infection preventionists over the last six months now have more experience than many of the policymakers up in D.C., because they’ve lived it firsthand. And they’ve seen how COVID-19 can spread. And they’re starting to develop a good idea of how to stop it.”

Perhaps now is the time that innovation begins to rely more heavily on infection preventionists and our valuable insight into the world of healthcare PPE. The changes we help guide now, can help make healthcare safer and infection prevention easier.

When COVID-19 struck, the proper use of PPE and greater attention to hand hygiene and cleaning surfaces became the norm. When that happened, rates of Clostridium difficile decreased significantly.
Sarah Smathers, MPH, CIC, FAPIC: “I think that hospital administrators are concerned about how they’re going to recruit in a field that is expecting a lot of retirees: 40% of infection professionists are expected to retire in the next five to 10 years.”

Devin Jopp, EdD, MS: “[W]e will work to elevate our collective voice to ensure infection prevention and control is at the core of our healthcare delivery system and woven into the very fabric of our community.”

COVID-19 possibly hindered the prevention of healthcare-acquired infections (HAIs) because infection preventionists have less time to do rounding and focus on the elements that contribute to HAIs.

Simply put, a single approach strategy, like the test-only approach within the White House, is one doomed for failure. Meanwhile, the CDC updates what it means by an airborne transmission of COVID-19.

Bilal Naseer, MD: “Nurses who are kind of at a point where they cannot do bedside care, they should consider infection prevention. We need more infection preventionists.”