News


Imagine swallowing a pill today that continues releasing the daily dose of a medicine you need for the next week, month or even longer. Investigators from Brigham and Women's Hospital and their collaborators from the Massachusetts Institute of Technology have developed a long-acting drug delivery capsule that may help to do just that in the future. To test the capsule's real-world applications, the team used both mathematical modeling and animal models to investigate the effects of delivering a sustained therapeutic dose of a drug called ivermectin, which is used to treat parasitic infections such as river blindness. Ivermectin has an added bonus of helping keep malaria-carrying mosquito populations at bay. The team found that in large animal models, the capsule safely stayed in the stomach, slowly releasing the drug for up to 14 days, and potentially providing a new way to combat malaria and other infectious diseases. The results of this work are published Nov. 16 in Science Translational Medicine.
Infectious diseases are a leading cause of mortality worldwide. The development of novel therapies or vaccines requires improved understanding of how viruses, pathogenic fungi or bacteria cause illnesses. Some bacterial pathogens such as Salmonella invade and replicate within human cells. Science is steadily shifting its focus towards studying infected cells and how differences between individual host cells affect the cellular response to pathogens.





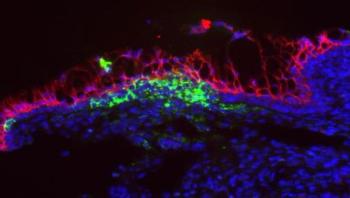
It sounds like the plot of a 1950s science fiction movie: normal, helpful bacteria that begin to eat their host from within, because they don’t get what they want. But new research shows that’s exactly what happens when microbes inside the digestive system don’t get the natural fiber that they rely on for food. Starved, they begin to munch on the natural layer of mucus that lines the gut, eroding it to the point where dangerous invading bacteria can infect the colon wall. In a new paper in Cell, an international team of researchers show the impact of fiber deprivation on the guts of specially raised mice. The mice were born and raised with no gut microbes of their own, then received a transplant of 14 bacteria that normally grow in the human gut. Scientists know the full genetic signature of each one, making it possible to track their activity over time.







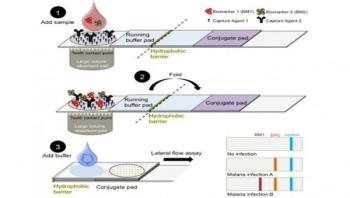
An interdisciplinary team of scientists and engineers at Vanderbilt University headed by Stevenson Professor of Chemistry David Wright has designed a new kind of rapid diagnostic test for malaria that has received a $100,000 Grand Challenges Explorations grant which is designed to support innovative global health and development research projects. It is one of 56 such grants announced today by the Bill & Melinda Gates Foundation.
Scientists at the Gladstone Institutes discovered that the vaginal immune system is suppressed in response to RNA viruses, such as Zika. The delayed antiviral immune response allows the virus to remain undetected in the vagina, which can increase the risk of fetal infection during pregnancy.

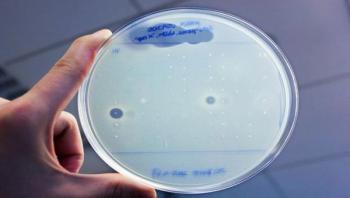
Most antibiotics in use today are based on natural molecules produced by bacteria--and given the rise of antibiotic resistance, there's an urgent need to find more of them. Yet coaxing bacteria to produce new antibiotics is a tricky proposition. Most bacteria won't grow in the lab. And even when they do, most of the genes that cause them to churn out molecules with antibiotic properties never get switched on.