
Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending March 11.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending March 11.
A comprehensive blueprint on how to be better prepared for the future as COVID-19 becomes endemic and the world faces future pandemics.

A new study supports the conclusion that the “brain fog” reported by many who have recovered from mild COVID-19 infection is real and has an anatomical basis.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending March 4.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending February 25.

Investigators used 3 behavior models to study how to increase health care workers’ compliance with infection prevention and control practices.

The goal of the review was to examine the efficacy of the World Health Organization’s 6-step handwashing technique and compare its efficacy with other handwashing techniques.

Bug of the Month helps educate readers about existing and emerging pathogens of clinical importance in healthcare facilities today.

Reinfections among study participants most likely occurred outside the hospital setting where workers might let their guard down and not practice nonpharmaceutical mitigation efforts against SARS-CoV-2.

The ability to be an excellent infection preventionist requires lifelong learning and taking the initiative to grow professionally.
Outpatient settings are not like inpatient settings. They have unique requirements and circumstances, including those related to infection prevention and control.

The successful combination of products and the adoption and application of science-based practices will help the sterile processing profession rise above challenges to protecting frontline technicians.
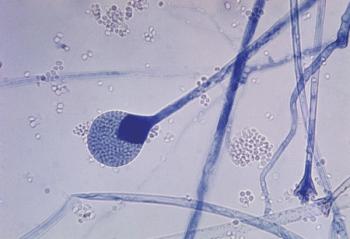
Bug of the Month helps educate readers about existing and emerging pathogens of clinical importance in healthcare facilities today.

There are many facets to creating smarter, healthier health care spaces through infection control and prevention, but these tips can help generate a cohesive, adaptable and curative plan.

Dental instruments may not seem as invasive as the instruments used in medical surgeries, but they still pose the same dangers.

Having an infection preventionist on site or as a consultant to lead infection prevention and control training makes a difference. The ability to screen, isolate, or group patients can save lives. Ongoing testing of residents and staff is critical.

La’Titia Houston MPH, BSN, RN, CIC: “We work not only with the bedside nurses and the sterile processors, but even with our clinicians, our physicians. They want a timeout before the procedure is even performed because they want to ensure that the scope did pass during the high-level disinfection procedure.”
Bug of the Month helps educate readers about existing and emerging pathogens of clinical importance in healthcare facilities today.

No health care worker is immune from the dangers of handling sharps. Physicians hold a rate just under that of nurses, mostly related to use of scalpels, but are less likely to report these injuries.

What does the post-COVID-19 future look like for infection preventonists? Great strides in infection prevention have been made because of the COVID-19 response, but look for them to be modified moving forward.

Adenosine triphosphate (ATP) bioluminescence needs technological enhancement if it’s to reach its full potential as a disinfection tool, says a study.

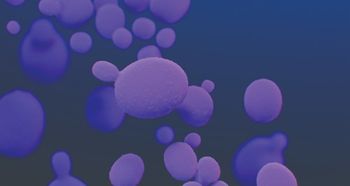
Doe Kley, RN, CIC, MPH,T-CHEST: “We just can’t keep doing what we’ve been doing with our singular focus on one pathogen. We know that while we were doing that—while we were so busy with COVID-19—other really dangerous and emerging pathogens got a foothold. The one that scares me the most is Candida auris.”

Darrel Hicks: “EVS teams work around professionals who are certified—whether it’s respiratory therapists, physical therapists, the RNs, the doctors—and I think if we ever hoped to elevate their status that we need to certify environmental services workers to a certain level of knowledge before they even start cleaning patient rooms.”
The use of almost every antibiotic increases the chances of Clostridioides difficile infection, and that includes the drugs that are used to treat C diff, a study states.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending October 29.